Urothelial Carcinoma (Transitional Cell Carcinoma)
Overview
Urothelial carcinoma (UC), formerly known as transitional cell carcinoma (TCC), is a malignant tumor arising from the urothelium — the specialized lining of the urinary tract that extends from the renal pelvis to the urethra.
It is the most common type of bladder cancer and can also occur in the ureters or renal pelvis (collectively called upper tract urothelial carcinoma, UTUC).
Urothelial carcinoma is often linked to tobacco exposure, chemical carcinogens, and chronic inflammation.
The disease ranges from superficial, non–muscle-invasive tumors to deeply invasive and metastatic disease, requiring different management approaches.
Symptoms
- Painless hematuria (blood in urine) — most common symptom
- Urinary frequency, urgency, or dysuria (painful urination)
- Pelvic or flank pain (in advanced disease)
- Fatigue, weight loss, or bone pain (metastatic spread)
- Occasionally detected incidentally on imaging
Causes & Risk Factors
- Smoking – leading cause (accounts for up to 50% of cases)
- Occupational exposure to aromatic amines (dyes, rubber, paint industries)
- Chronic bladder irritation (long-term catheters, stones, schistosomiasis)
- Prior chemotherapy (especially cyclophosphamide) or pelvic radiation
- Genetic predisposition: Lynch syndrome (HNPCC) increases risk of upper tract UC
- More common in men and in older adults (ages 60–80)
Diagnosis
- Urinalysis & cytology: Detects hematuria and malignant cells
- Cystoscopy: Gold standard for bladder visualization and biopsy
- Imaging:
- CT urography – evaluates entire urinary tract for masses
- MRI or ultrasound – alternative imaging options
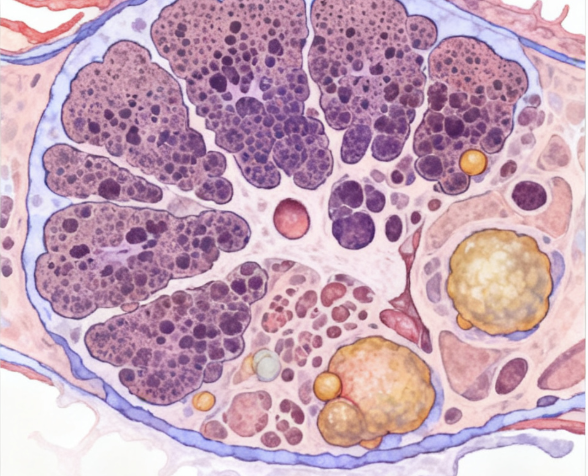
- Histopathology:
- Confirms urothelial origin and tumor grade (low vs. high)
- Determines invasion depth (non–muscle-invasive vs. muscle-invasive)
- Molecular testing: Identifies mutations (FGFR3, TP53, TERT) for prognosis or targeted therapy
- Staging: Based on TNM system (extent of invasion, lymph node, and metastasis)
Treatment Options
- Non–muscle-invasive disease (Ta, T1, CIS):
- Transurethral resection of bladder tumor (TURBT)
- Intravesical therapy: Bacillus Calmette-Guérin (BCG) or mitomycin C
- Regular cystoscopic surveillance for recurrence
- Muscle-invasive disease (T2–T4):
- Radical cystectomy (bladder removal) ± urinary diversion
- Neoadjuvant chemotherapy: Cisplatin-based (MVAC or gemcitabine-cisplatin)
- Bladder-sparing protocols: Chemoradiation in selected patients
- Metastatic disease:
- Systemic chemotherapy: Cisplatin-based regimens
- Immunotherapy: PD-1/PD-L1 inhibitors (pembrolizumab, nivolumab, atezolizumab)
- Targeted therapy: FGFR3 inhibitors (erdafitinib) for specific mutations
- Clinical trials: Ongoing research in personalized immuno-oncology
Prognosis
- Non–muscle-invasive disease: Excellent prognosis with proper surveillance (5-year survival ~90%)
- Muscle-invasive disease: Intermediate prognosis; 5-year survival ~50% after radical surgery
- Metastatic disease: Poor prognosis (median survival ~12–18 months with systemic therapy)
- Key prognostic factors: Tumor stage, grade, multifocality, and recurrence rate
- Lifelong surveillance needed due to high recurrence risk
Living with this Cancer Type
- Frequent cystoscopy and urine tests to monitor recurrence
- Lifestyle adjustments: Smoking cessation, hydration, diet modification
- Rehabilitation: Adapting to urinary diversion or neobladder after cystectomy
- Psychosocial support: Coping with body image and quality of life changes
- Regular follow-up: Imaging, lab work, and renal function monitoring
- Access to support groups for bladder cancer survivors
Prevention & Screening
- Quit smoking: Most effective preventive measure
- Occupational protection: Avoid exposure to aromatic amines, dyes, and chemicals
- Early medical evaluation: For any visible blood in urine
- Surveillance protocols: For patients with previous bladder tumors or high-risk occupations
- Genetic testing: In Lynch syndrome families for upper tract surveillance
FAQs
Q: Is urothelial carcinoma the same as bladder cancer?
A: Yes, most bladder cancers are urothelial carcinomas, but the same type can also occur in the ureter or renal pelvis.
Q: Can urothelial carcinoma come back after treatment?
A: Yes. It has one of the highest recurrence rates among cancers, especially in non–muscle-invasive forms, which is why lifelong monitoring is essential.
Q: Is it hereditary?
A: Most cases are not hereditary, though Lynch syndrome slightly increases the risk.
Q: Can it be cured?
A: Early-stage and localized cases are often curable with resection and intravesical therapy. Advanced cases are treatable but not always curable.
Resources
- American Cancer Society (ACS) – cancer.org
- Bladder Cancer Advocacy Network (BCAN) – www.bcan.org
- National Cancer Institute (NCI) – cancer.gov
- European Association of Urology (EAU) – uroweb.org
- gov – Search “Urothelial Carcinoma” or “Transitional Cell Carcinoma”
Understand Precision Testing
Learn how liquid biopsy and chemo sensitivity testing can personalize your treatment plan.
Make Informed Decisions
Gain knowledge to actively participate in treatment discussions with your healthcare team.
Improve Treatment Outcomes
Discover how precision medicine and metabolic therapies can enhance treatment effectiveness.
Start Your Educational Journey Today
Empower yourself with knowledge about precision metabolic oncology and take an active role in your cancer care journey.
Need More Information?
Our team of oncology experts is here to help you understand your diagnosis and treatment options.
