Kidney Cancer (Renal Cell Carcinoma)
Overview
Kidney cancer, also known as Renal Cell Carcinoma (RCC), is the most common type of kidney cancer in adults, accounting for about 90% of all malignant renal tumors.
It originates from the renal tubular epithelial cells within the nephron.
The main subtypes include:
- Clear Cell RCC (~75–80%)
- Papillary RCC (~10–15%)
- Chromophobe RCC (~5%)
- Collecting duct carcinoma and Medullary carcinoma (rare, aggressive variants)
Kidney cancer typically occurs between ages 50–70 years and is more common in men.
Early-stage disease often causes few or no symptoms and is sometimes discovered incidentally on imaging.
Symptoms
- Hematuria (blood in urine) – most common presenting sign
- Flank or side pain
- Palpable mass in the abdomen or flank
- Unexplained weight loss or fatigue
- Fever or night sweats (paraneoplastic)
- High blood pressure (hypertension)
- Anemia or polycythemia (due to altered erythropoietin production)
- Bone pain or cough in metastatic cases
(Note: The “classic triad” of hematuria, flank pain, and palpable mass occurs in <10% of modern cases.)
Causes & Risk Factors
- Smoking – major preventable risk factor
- Obesity and high blood pressure
- Chronic kidney disease or dialysis history
- Genetic syndromes:
- Von Hippel–Lindau (VHL) disease – associated with clear cell RCC
- Hereditary papillary RCC (MET gene mutations)
- Birt–Hogg–Dubé syndrome – linked to chromophobe RCC
- Tuberous sclerosis (rare association)
- Occupational exposure – to cadmium, trichloroethylene, or petroleum products
- Male sex and older age
Diagnosis
- Imaging:
- Ultrasound – initial screening tool for renal mass
- CT or MRI of abdomen and pelvis – defines size, location, and venous invasion
- Chest CT – checks for lung metastases
- Bone scan / PET-CT – if symptoms suggest metastasis
- Laboratory tests: CBC, renal and liver function, calcium, erythropoietin levels
- Histopathology: Confirms subtype and grade via biopsy or surgical specimen
- Staging: Based on TNM system (Tumor, Node, Metastasis)
Treatment Options
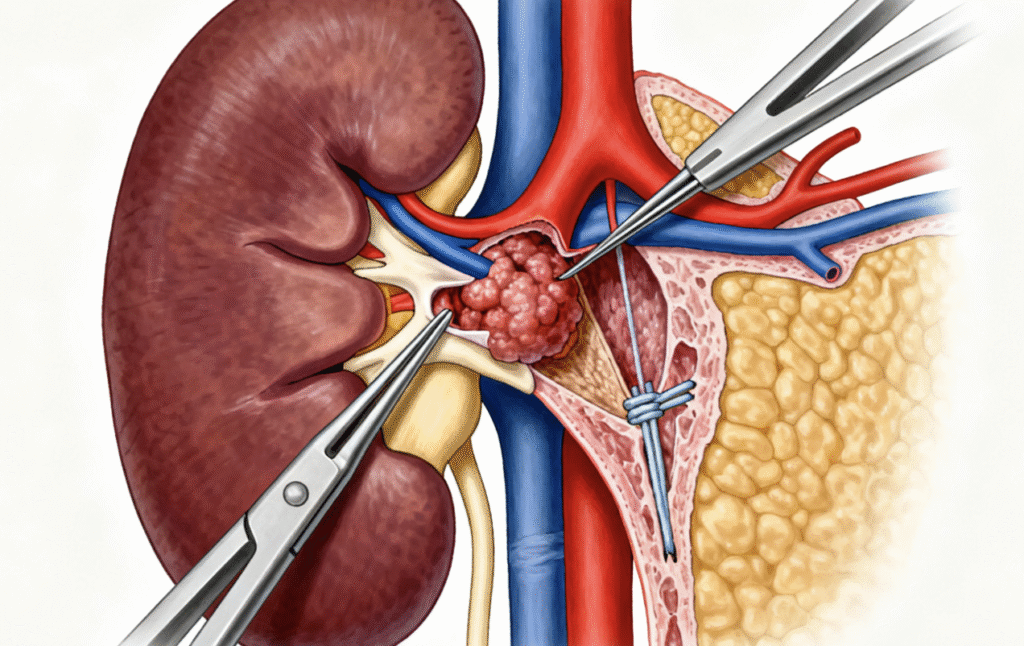
- Localized disease (Stage I–II):
- Partial nephrectomy (nephron-sparing surgery) for small tumors (<4 cm)
- Radical nephrectomy (removal of kidney ± adrenal gland) for larger or central tumors
- Locally advanced or metastatic disease (Stage III–IV):
- Targeted therapy:
- VEGF inhibitors (sunitinib, pazopanib, axitinib)
- mTOR inhibitors (everolimus, temsirolimus)
- Immunotherapy:
- Immune checkpoint inhibitors (nivolumab, pembrolizumab, ipilimumab)
- Combination regimens: Immunotherapy + targeted therapy (current standard of care)
- Ablation or embolization: For patients unfit for surgery
- Radiation therapy: For palliation of metastases (e.g., bone, brain)
- Targeted therapy:
- Clinical trials: Ongoing research in novel immunotherapy and personalized medicine (e.g., HIF-2α inhibitors).
Prognosis
- Localized RCC: 5-year survival rate ≈ 90–95% after surgery
- Locally advanced (stage III): 5-year survival ≈ 60–70%
- Metastatic (stage IV): Median survival ≈ 18–24 months with modern therapies
- Prognostic factors: Stage, histologic subtype, performance status, and molecular features (e.g., VHL status)
- Regular surveillance: Imaging every 6–12 months post-treatment for recurrence detection
Living with this Cancer Type
- Long-term monitoring: Periodic imaging, blood work, and kidney function tests
- Lifestyle adjustments: Quit smoking, maintain healthy weight, control blood pressure
- Nutrition and hydration: To preserve remaining kidney function
- Psychosocial support: Coping with anxiety, fatigue, and treatment side effects
- Rehabilitation and survivorship programs: For recovery and quality of life
- Fertility and sexual health counseling: If receiving targeted or immunotherapy
Prevention & Screening
- Avoid smoking and reduce exposure to industrial carcinogens
- Maintain healthy weight and blood pressure
- Regular check-ups for individuals with family history or genetic syndromes
- Genetic counseling and testing for VHL, Birt–Hogg–Dubé, or hereditary papillary RCC
- Imaging surveillance for high-risk patients (e.g., VHL carriers)
FAQs
Q: Is kidney cancer always fatal?
A: No. When detected early, kidney cancer is often curable with surgery. Advanced cases can be controlled for years with modern targeted and immunotherapies.
Q: Can kidney cancer spread to other organs?
A: Yes. Common metastatic sites include the lungs, bones, liver, and brain.
Q: Is it hereditary?
A: Most cases are sporadic, but around 2–4% are hereditary.
Q: Can a person live with one kidney?
A: Yes. Most people live normal, healthy lives after removal of one kidney, provided the other is functioning well.
Resources
- American Cancer Society (ACS) – cancer.org
- National Cancer Institute (NCI) – cancer.gov
- Kidney Cancer Association (KCA) – kidneycancer.org
- European Association of Urology (EAU) – uroweb.org
- gov – Search “Renal Cell Carcinoma” or “Kidney Cancer”
Understand Precision Testing
Learn how liquid biopsy and chemo sensitivity testing can personalize your treatment plan.
Make Informed Decisions
Gain knowledge to actively participate in treatment discussions with your healthcare team.
Improve Treatment Outcomes
Discover how precision medicine and metabolic therapies can enhance treatment effectiveness.
Start Your Educational Journey Today
Empower yourself with knowledge about precision metabolic oncology and take an active role in your cancer care journey.
Need More Information?
Our team of oncology experts is here to help you understand your diagnosis and treatment options.
