Juvenile Granulosa Cell Tumor (JGCT)
Overview
Juvenile Granulosa Cell Tumor (JGCT) is a rare ovarian sex cord–stromal tumor that originates from the granulosa cells of the ovary, which normally produce estrogen.
It represents the juvenile subtype of granulosa cell tumors, typically affecting children, adolescents, and young women under 30 years of age.
JGCT accounts for 5–10% of all granulosa cell tumors and <1% of all ovarian cancers.
Unlike the adult form, JGCT often presents with hormone-related symptoms (due to estrogen excess) and tends to be less aggressive. Most cases are unilateral and stage I at diagnosis.
Symptoms
- Abdominal swelling or pain (due to ovarian mass)
- Menstrual irregularities – amenorrhea, precocious puberty, or postmenopausal bleeding
- Breast tenderness or enlargement (estrogen excess)
- Early puberty in children (premature breast development, uterine bleeding)
- Pelvic pressure or urinary frequency (large tumors)
- Rarely: Ascites or acute abdomen (from rupture or torsion)
Causes & Risk Factors
● Largely sporadic; no established environmental or lifestyle risk factors
● Genetic mutations:
○ FOXL2 mutations common in adult-type granulosa cell tumors, but absent in JGCT
○ JGCT may show AKT1 or GNAS mutations in some cases
● Hormonal dysregulation – excessive estrogen production by tumor cells
● No strong hereditary pattern reported
● Peak incidence: Children and young adults (<30 years old)
Diagnosis
- Physical exam: Palpable adnexal (ovarian) mass or abdominal distension
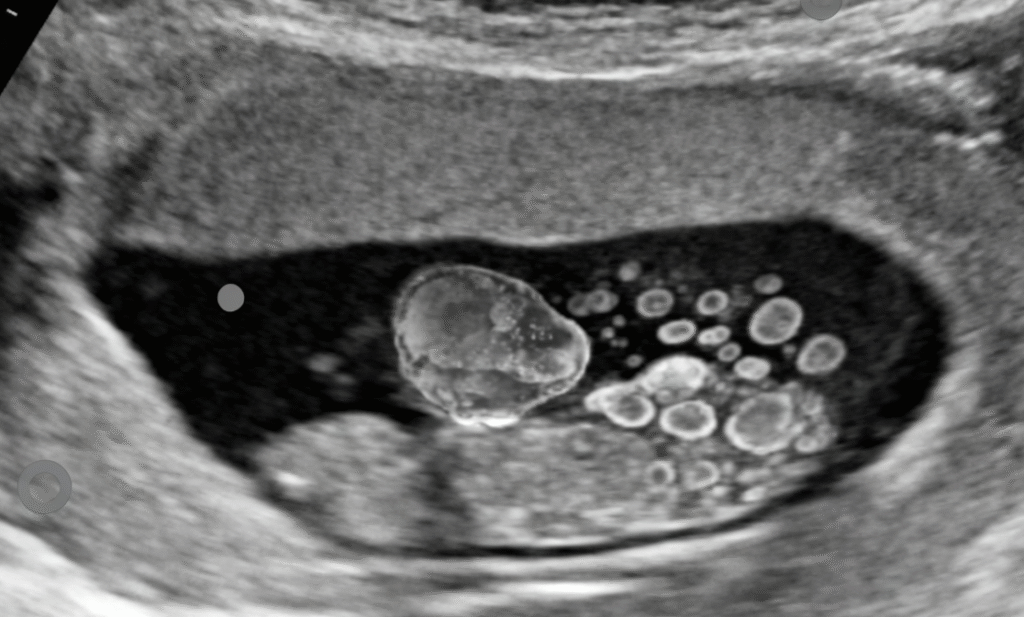
- Imaging:
- Pelvic ultrasound: Solid-cystic ovarian mass, often unilateral
- CT/MRI abdomen and pelvis: For tumor size, ascites, or spread assessment
- Laboratory findings:
- Elevated serum inhibin A/B or estradiol (hormonal markers)
- Tumor markers (CA-125, AFP) typically normal
- Histopathology:
- Follicle-like structures resembling immature follicles (“Call-Exner bodies” uncommon in juvenile type)
- High mitotic activity compared with adult form
- Staging: Based on FIGO ovarian cancer system
Treatment Options
- Surgery:
- Unilateral salpingo-oophorectomy (removal of affected ovary and tube) is the standard treatment for Stage I disease.
- Fertility-sparing surgery preferred in young patients.
- Comprehensive staging: Peritoneal washings, omental biopsy, inspection of contralateral ovary.
- Chemotherapy:
- Indicated for advanced, recurrent, or high-grade tumors.
- Common regimens: BEP (Bleomycin, Etoposide, Cisplatin) or Carboplatin + Paclitaxel.
- Radiation therapy: Rarely used, reserved for palliative settings.
- Clinical trials: Limited but ongoing for hormonal and targeted therapies (anti-estrogen agents).
Prognosis
- Excellent prognosis for early-stage (Stage I) disease; 5-year survival >95%.
- Recurrence risk: 5–10%, usually within 3–5 years of treatment.
- Advanced-stage disease: Worse prognosis but still more favorable than epithelial ovarian cancers.
- Key prognostic factors: Tumor stage, rupture, mitotic index, and completeness of surgical removal.
- Long-term follow-up: Required for up to 10–15 years due to potential late recurrences.
Living with this Cancer Type
- Regular follow-up: Pelvic exams, ultrasound, and serum inhibin/estradiol monitoring every 3–6 months.
- Fertility preservation: Many patients retain fertility after unilateral surgery.
- Hormonal balance: Estrogen levels normalize post-surgery; menses typically resume.
- Psychosocial support: For young patients coping with early diagnosis and surgical outcomes.
- Education: Awareness of recurrence signs (abdominal pain, irregular bleeding).
Prevention & Screening
- No known prevention due to sporadic nature.
- Routine gynecologic checkups and pelvic imaging if hormonal symptoms occur.
- Genetic counseling if strong family history of ovarian tumors, though inheritance is rare.
- Education for pediatricians and gynecologists: Early recognition of hormone-related signs in children.
FAQs
Q: Is Juvenile Granulosa Cell Tumor cancerous?
A: Yes, it is malignant, but typically low-grade and slow-growing with high curability when detected early.
Q: Can it affect fertility?
A: Most patients retain fertility since the disease is usually unilateral and treated conservatively.
Q: Can it recur after treatment?
A: Recurrence is rare but possible; ongoing follow-up for 10–15 years is recommended.
Q: What’s the difference between juvenile and adult granulosa cell tumors?
A: Juvenile type occurs in younger patients, lacks FOXL2 mutation, shows higher mitotic activity, and has a slightly different microscopic appearance.
Resources
- National Cancer Institute (NCI) – cancer.gov
- American Cancer Society (ACS) – cancer.org
- Children’s Oncology Group (COG) – childrensoncologygroup.org
- Ovarian Cancer Research Alliance (OCRA) – ocrahope.org
- gov – Search “Juvenile Granulosa Cell Tumor”
Understand Precision Testing
Learn how liquid biopsy and chemo sensitivity testing can personalize your treatment plan.
Make Informed Decisions
Gain knowledge to actively participate in treatment discussions with your healthcare team.
Improve Treatment Outcomes
Discover how precision medicine and metabolic therapies can enhance treatment effectiveness.
Start Your Educational Journey Today
Empower yourself with knowledge about precision metabolic oncology and take an active role in your cancer care journey.
Need More Information?
Our team of oncology experts is here to help you understand your diagnosis and treatment options.
