- +852 4750 3485
- info@mycancerinfo.org
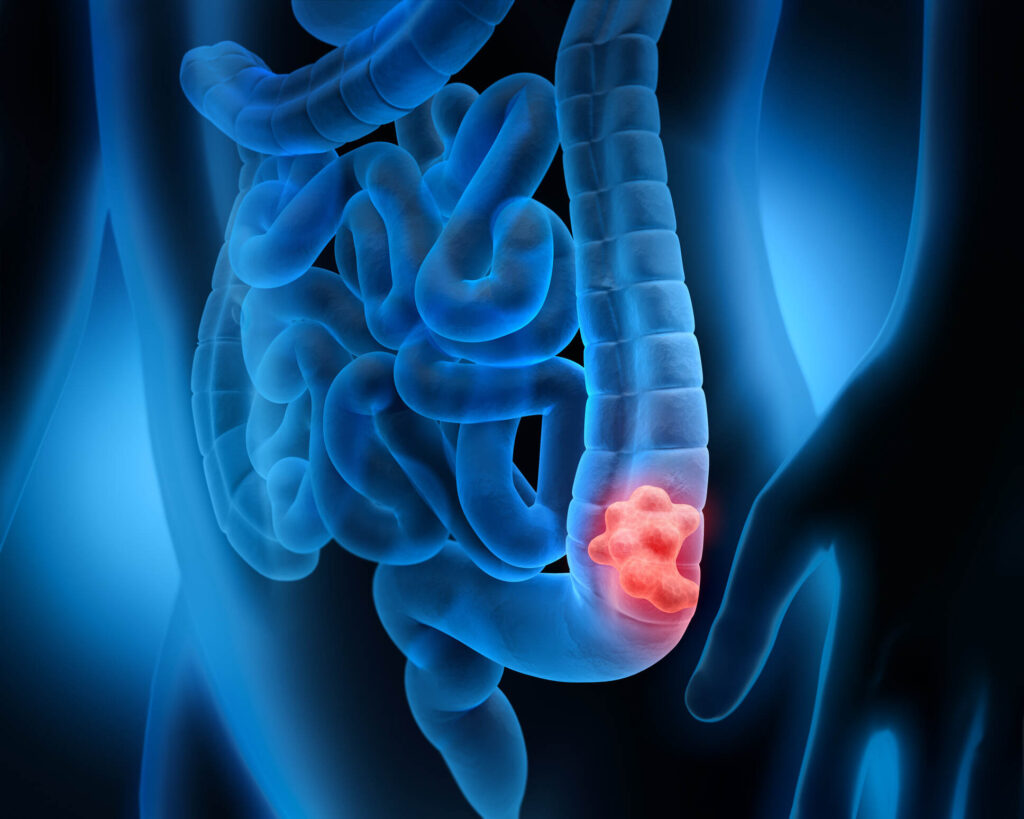
A colonoscopy is a medical procedure that allows doctors to examine the inside of the large intestine (colon and rectum) using a long, flexible tube with a camera and light (a colonoscope).
It is considered the gold standard screening test for colorectal cancer because it can both detect and prevent cancer by identifying and removing precancerous polyps during the same procedure.
Learn how liquid biopsy and chemo sensitivity testing can personalize your treatment plan.
Gain knowledge to actively participate in treatment discussions with your healthcare team.
Discover how precision medicine and metabolic therapies can enhance treatment effectiveness.
Empower yourself with knowledge about precision metabolic oncology and take an active role in your cancer care journey.
Our team of oncology experts is here to help you understand your diagnosis and treatment options.